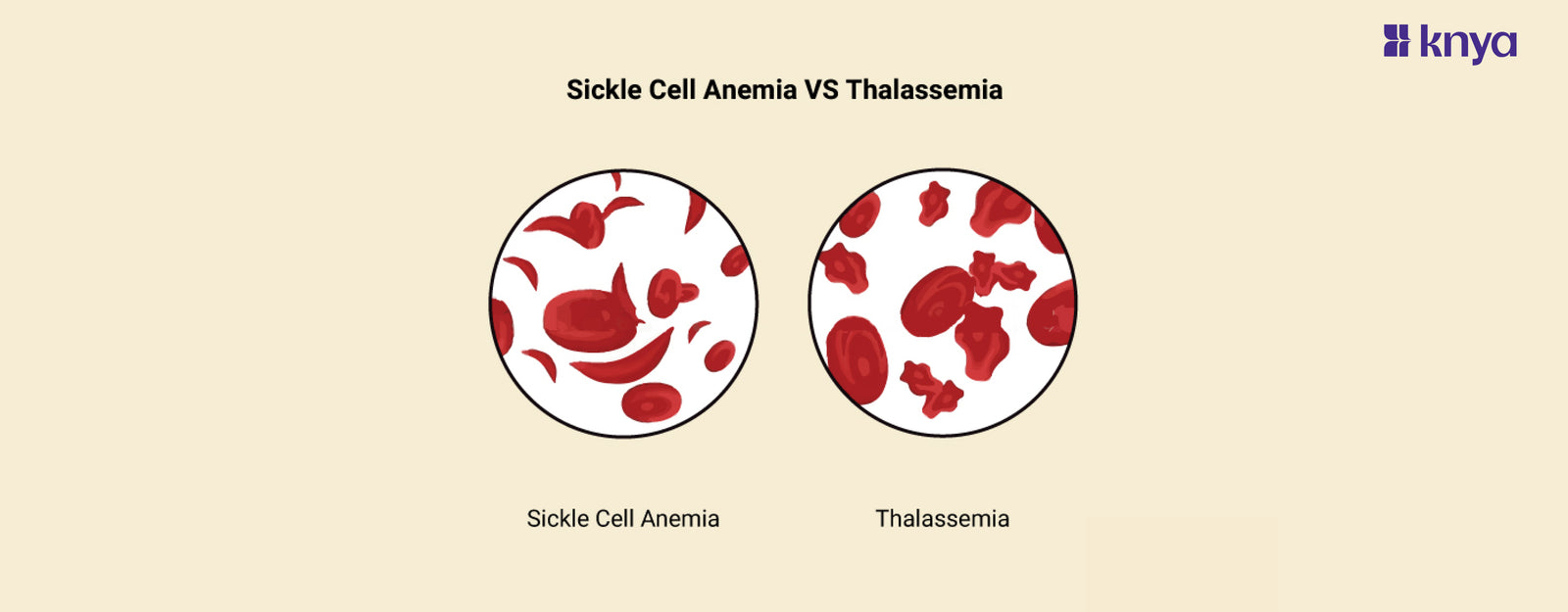
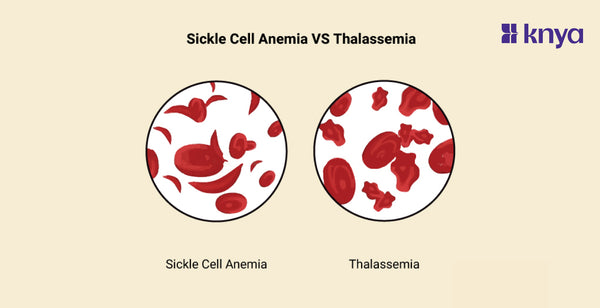
Difference Between Sickle Cell Anemia and Thalassemia: Sickle Cell Anemia and Thalassemia are hereditary blood illnesses that affect haemoglobin (Hb) and cause anaemia; however, their causes and cardiac consequences are different. Sickle Cell Anaemia is characterised by a mutant, "sickle-shaped" red blood cell that clogs arteries, causing a vaso-occlusive crisis and potentially damaging the heart muscle. In contrast, thalassemia is characterised by inadequate haemoglobin production, resulting in persistent anaemia and iron overload. This excess can accumulate in the heart, resulting in cardiomyopathy and arrhythmia. Though both illnesses pose cardiac concerns, their treatment differs, emphasising the critical distinction between Sickle Cell Anemia and Thalassemia.
[image_banner]
Difference Between Sickle Cell Anemia and Thalassemia
Sickle Cell Anemia and Thalassemia are both genetic disorders that affect the production of hemoglobin, the protein in red blood cells responsible for carrying oxygen. Highlighting the differences between Sickle Cell Anemia and Thalassemia
|
Feature |
Sickle Cell Anemia |
Thalassemia |
|
Underlying Genetic Mutation |
HBB gene mutation (Hemoglobin S - HbS) |
HBA1, HBA2, or HBB gene mutations |
|
Type of Hemoglobin Produced |
Abnormal hemoglobin S (HbS) causes sickle-shaped cells |
Reduced or absent production of normal hemoglobin |
|
Inheritance Pattern |
Autosomal recessive |
Autosomal recessive (or dominant, depending on type) |
|
Geographical Distribution |
More prevalent in malaria-endemic regions |
Found in regions like the Mediterranean, Southeast Asia, and parts of Africa |
|
Clinical Symptoms |
Pain crises, anemia, organ damage, susceptibility to infections |
Anemia, fatigue, jaundice, potential for bone deformities and organ damage |
|
Severity of Disease |
Variable severity, ranging from mild to severe |
Variable severity, ranging from mild to severe |
|
Red Blood Cell Lifespan |
Shortened lifespan due to abnormal shape (hemolysis) |
Reduced production leads to premature destruction (hemolysis) |
|
Treatment Approaches |
Pain management, hydration, blood transfusions, bone marrow transplantation |
Blood transfusions, iron chelation, bone marrow transplantation |
|
Malaria Resistance |
Provides some resistance to malaria |
Does not provide the same level of resistance to malaria |
|
Effect on Oxygen Delivery |
Impaired oxygen delivery during sickling episodes |
Decreased oxygen-carrying capacity |
Browse Best Scrubs Collection
What is Sickle Cell Anemia?
Sickle cell anemia is a hereditary blood condition in which faulty hemoglobin molecules cause red blood cells to form a crescent shape. These cells get lodged in blood arteries, obstructing oxygen flow and causing discomfort, exhaustion, organ damage, and an increased risk of infection. Most persons of African heritage inherit it from both parents. Treatments are intended to control symptoms, avoid complications, and enhance quality of life.
Key Features of Sickle Cell Anemia:
- Individuals with sickle cell anaemia inherit a mutant type of haemoglobin known as haemoglobin S. This protein, which is essential for oxygen delivery, becomes hard and sticky in low oxygen circumstances, causing red blood cells to sickle (take on a crescent shape).
- Sickled red blood cells are less flexible and tend to clump, blocking tiny blood arteries. This obstruction impairs oxygen transport to tissues, resulting in discomfort, tissue damage, and organ malfunction.
- Sickled cells have a shorter lifespan, resulting in an ongoing scarcity of healthy red blood cells. This deficit, known as anaemia, produces weariness, weakness, and shortness of breath.
- Individuals with sickle cell anaemia are more prone to infections due to impaired spleen function, strokes caused by blocked blood vessels in the brain, and delayed growth and development due to inadequate oxygen supply.
[image_banner]
What is Thalassemia?
Thalassemia is another genetic blood condition that impairs hemoglobin synthesis. Depending on the kind, either the alpha or beta globin protein chains in hemoglobin are decreased, resulting in fewer and smaller red blood cells. This results in anaemia, weariness, weakness, and even organ damage. It is also handed down via parents and is especially common among Mediterranean, Middle Eastern, and Southeast Asian communities. Treatments are aimed at symptom management and preventing complications; in extreme instances, blood transfusions and bone marrow transplants may be necessary.
Key Features of Thalassemia:
- Thalassemia involves mutations in genes responsible for globin production, a key component of hemoglobin. This leads to less hemoglobin being produced, ultimately reducing the oxygen-carrying capacity of red blood cells.
- Due to insufficient hemoglobin, red blood cells in Thalassemia are smaller and pale (microcytic). This results in anemia similar to Sickle Cell Anemia, causing fatigue, weakness, and shortness of breath.
- Thalassemia exists in various forms, ranging from mild (thalassemia trait) to severe (thalassemia major). The severity depends on the specific gene mutations inherited and the amount of hemoglobin produced.
- Depending on the type and severity, Thalassemia can lead to bone deformities due to bone marrow expansion, iron overload from frequent blood transfusions, and heart problems due to increased workload on the heart.
Shop Best Lab Coats from Here!
Similarities Between Sickle Cell Anemia and Thalassemia
- Genetic Basis: Both Sickle Cell Anemia and Thalassemia are inherited genetic disorders caused by mutations in specific genes involved in hemoglobin production.
- Anemia: Both disorders are characterized by anemia, a condition where there is a reduced number of red blood cells or a decreased amount of hemoglobin in the blood.
- Chronic Conditions: Both Sickle Cell Anemia and Thalassemia are chronic conditions that require long-term management and care.
- Risk of Complications: Both disorders are associated with an increased risk of complications, such as organ damage, infections, and impaired quality of life.
- Inherited Recessively: Inheritance of both disorders follows an autosomal recessive pattern, meaning that an affected individual has inherited two copies of the mutated gene (one from each parent).
Sickle Cell Anemia and Thalassemia are both hereditary blood illnesses that affect red blood cells; however, their underlying processes and consequences are very different. Sickle Cell Anemia is caused by a single gene mutation that causes sickle-shaped red blood cells that obstruct blood flow. Thalassemia, on the other hand, is caused by a combination of gene changes that impact either hemoglobin synthesis or structure, resulting in smaller and less efficient red blood cells. This difference leads to various symptoms. Sickle Cell Anaemia is characterised by painful bouts and organ damage, whereas Thalassemia produces severe anaemia and lethargy. Treatment techniques also differ, with Sickle Cell Anaemia emphasising pain management and avoiding complications, whilst Thalassemia frequently requires blood transfusions and iron chelation treatment.
| Check out More Articles | |
| Difference Between Cartilage and Bone | |
| Difference Between Endocrine and Exocrine Glands | |
| Difference Between Cell Wall and Cell Membrane | |