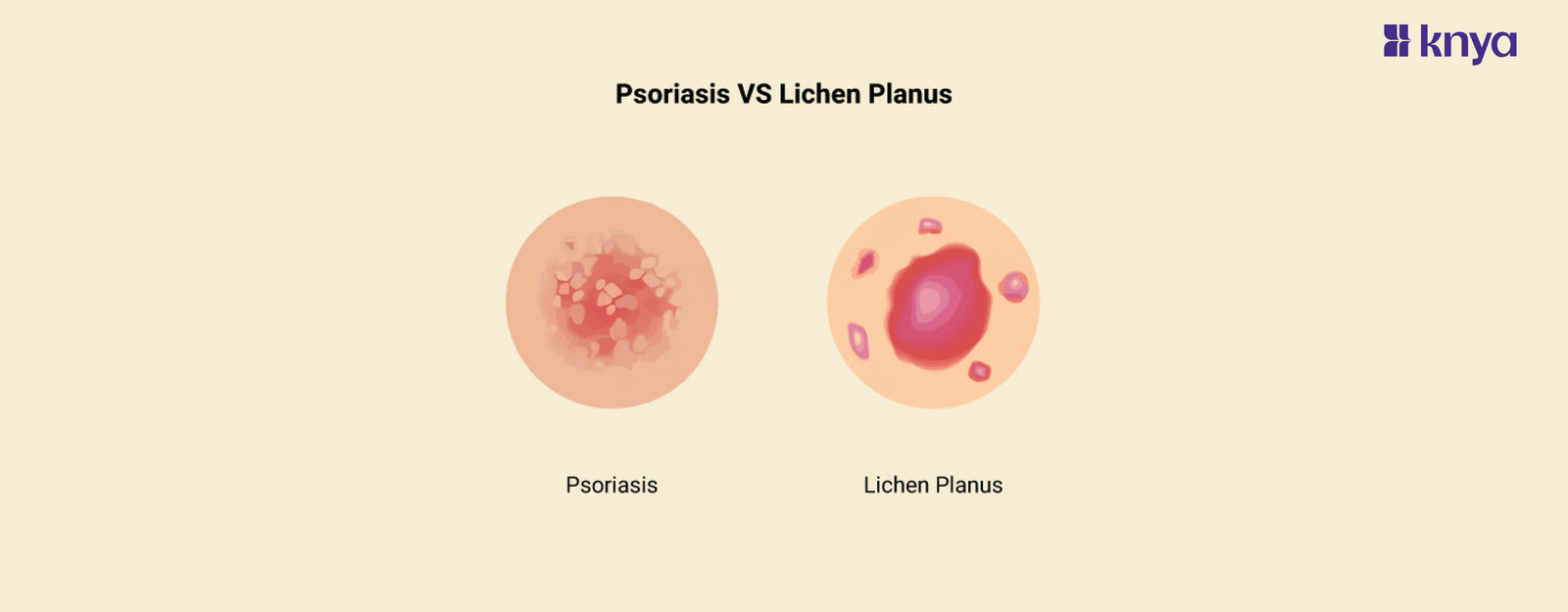
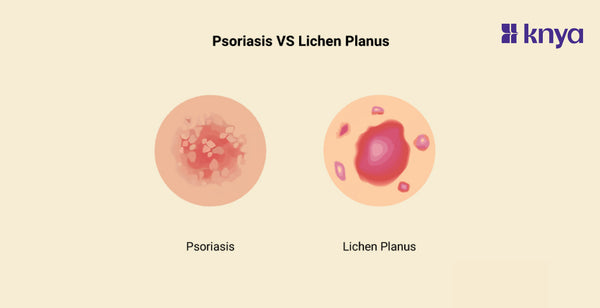
Difference Between Psoriasis and Lichen Planus: Both psoriasis and lichen planus can create itchy, scaly areas on the skin, but they differ in their origin, appearance, and treatment. Psoriasis, which is likely caused by an overactive immune system, causes thick, red plaques on the elbows, knees, scalp, and lower back, whereas lichen planus, which may be caused by stress or allergies, causes tiny, flat-topped purple lumps on the wrists, inner arms, and legs. While both may be treated with topical creams and lifestyle modifications, psoriasis may necessitate further treatments such as light therapy or medicines.
Psoriasis:
- Thickened plaques on the elbows, knees, scalp, and other regions, typically coated with silvery scales.
- Itchy and swollen: Burning, stinging, and pain may occur.
- Symptoms wax and wane in response to stress, illnesses, or certain drugs.
- Autoimmune link: Caused by an overactive immune system that attacks skin cells by mistake.
Lichen Planus:
- Flat-topped bumps: Purple or reddish-brown, with a waxy sheen, that occur on the wrists, ankles, and inside the lips.
- Itching is intense and disrupts sleep and daily life.
- Borders are clear and well-defined, as opposed to the hazy borders of psoriasis.
- Less frequently used: It is less common than psoriasis and can cause hair loss and nail problems.
Difference Between Psoriasis and Lichen Planus:
Psoriasis and Lichen Planus are both severe skin disorders, however, they have unique characteristics. Let's decode the differences between Psoriasis and Lichen Planus.
|
Feature |
Psoriasis |
Lichen Planus |
|
1. Type of Skin Condition |
Chronic autoimmune disorder |
Immune-mediated inflammatory disorder |
|
2. Cause |
Genetic and environmental factors contribute |
Autoimmune reaction or allergic response |
|
3. Lesion Appearance |
Red, raised, scaly plaques |
Flat-topped, purplish, polygonal papules |
|
4. Itching Severity |
Can be intense and vary in severity |
Often itchy, especially in the acute phase |
|
5. Location on Body |
Common on elbows, knees, scalp, and lower back |
Common on wrists, ankles, lower legs, and mucous membranes |
|
6. Nail Involvement |
Common; may cause pitting, discoloration |
Less common; may cause longitudinal ridges |
|
7. Mucous Membrane Involvement |
Rare |
Common, particularly in oral Lichen Planus |
|
8. Koebner Phenomenon |
Common; new lesions forming at sites of injury or trauma |
Less common but can occur |
|
9. Age of Onset |
Typically occurs between 15 and 35 years |
More common in middle-aged adults |
|
10. Triggers |
Stress, infections, and certain medications |
Drugs, hepatitis C infection, stress |
What is Psoriasis?
Psoriasis paints the skin in red and scaly patches, often triggered by stress, weather changes, or infections. Its relentless proliferation of skin cells builds thick, flaky plaques, most commonly on elbows, knees, scalp, and the lower back. While not contagious, it can flare unpredictably, impacting both physical comfort and emotional well-being.
Causes of Psoriasis:
- Immune System Overdrive in your immune system kills healthy skin cells by mistake, resulting in rapid growth and scaling.
- Genetic Connection of Having psoriasis in your family raises your risk.
- Environmental triggers include stress, illnesses, certain drugs, and even the weather.
- Skin Injuries like cuts, scratches, and sunburns can cause new psoriatic patches to appear.
- Obesity and metabolic problems, such as diabetes, may play a role.
- Smoking and drinking may worsen psoriasis symptoms.
Symptoms of Psoriasis:
- Red, elevated patches: These can occur on the elbows, knees, scalp, and other regions and are often coated with silvery scales.
- Itching: From moderate to severe, persistent scratching can aggravate lesions and create discomfort.
- Changes in fingernails and toenails include pitting, colour change, and crumbling.
- Painful and swollen joints might accompany skin symptoms in certain circumstances, particularly with psoriatic arthritis.
- Small, red, teardrop-shaped lesions may feel hot and sensitive, especially if you have digestive psoriasis.
Key characteristics of Psoriasis:
- Lesion Appearance: Red, raised plaques covered with silver-white scales.
- Itching: Itching can range from mild to severe.
- Nail Involvement: Common; may cause pitting, discoloration, and thickening of nails.
- Mucous Membrane Involvement: Typically absent, but can occur in some cases.
- Koebner Phenomenon: Common; new lesions may appear at sites of injury or trauma.
- Age of Onset: Typically starts between 15 and 35 years.
- Triggers: Triggers include stress, infections, and certain medications.
While psoriasis may be difficult to live with, with its unpredictable flare-ups and obstinate spots, it's vital to remember that disease doesn't define who you are. You may retake control and negotiate life with confidence if you have proactive management, effective therapies, and a supporting network. Remember, underneath the scales resides a resilient soul eager to enjoy a bright and fulfilling life.
What is Lichen Planus?
Lichen planus is a mystery engraved on the skin, with its unique violet-tinged, flat-topped lumps. Its origin is unknown, however stress and autoimmune responses are suggested. It can affect any part of the body, including the delicate folds of the lips and genitals, as well as the sun-kissed arms and legs. While it is less common than psoriasis, its itchy, burning lesions may be just as uncomfortable
Causes of Lichen Planus:
- The precise reason is unknown: We're still stumped as to who the real culprit is.
- Immune system malfunction: It's possible that your immune system is wrongly attacking skin and mucous membrane cells.
- Family history may have a role, indicating inherited susceptibilities.
- Stress and trauma: Emotional upheaval can occasionally precipitate or exacerbate flares.
- Some viruses, such as hepatitis C, may be implicated in viral infections.
- Medications: Certain medications, such as gold salts, might cause lichenoid responses.
- Allergies: Contact with certain metals or chemicals is uncommon.
Symptoms of Lichen Planus:
- Itchy, flat, purple patches: These can occur on the skin, scalp, nails, or even mucous membranes like the mouth and genitals and are commonly accompanied by noticeable white streaks.
- Burning or stinging sensation: Affected regions might be painful and sensitive, resulting in burning or stinging feelings.
- Nail involvement is prevalent, resulting in nails that are weak, discoloured, or even pitted and disintegrating.
- Blisters or erosions: In extreme cases, blisters or erosions may form, particularly in the mouth or genital regions.
- Hair loss: Scalp lichen planus can cause patchy hair loss, leaving lifelong scars.
Key characteristics of Lichen Planus:
- Lesion Appearance: Flat-topped, purplish, polygonal papules often forming a network.
- Itching: Often itchy, especially during the acute phase.
- Nail Involvement: Less common; may cause longitudinal ridges.
- Mucous Membrane Involvement: Common, particularly in oral Lichen Planus affecting the mouth and genitals.
- Koebner Phenomenon: Less common but can occur.
- Age of Onset: More common in middle-aged adults.
- Triggers: Triggers include drugs, hepatitis C infection, and stress.
With its scratchy patches and careful balance, lichen planus might feel like a permanent friend. But keep in mind that you are not alone on this path. You may minimise the itch, calm the lesions, and discover methods to live peacefully with this disease with careful skincare, suitable therapies, and a conscious attitude. Embrace your inner power and find the beauty that lies beyond the purple streaks, for there is a vivid world waiting to be explored with confidence and elegance.
Similarities between Psoriasis and Lichen Planus:
While psoriasis and lichen planus are separate skin disorders, they have shocking parallels apart from painful, red spots.
- Skin Deep: Both primarily affect the skin, causing raised, inflamed lesions that can be itchy and uncomfortable.
- Trigger Happy: Both can be triggered by stress, infections, certain medications, and even some environmental factors.
- Patchwork Quilt: Both form distinct patches on the skin, though their textures and patterns may differ. (Psoriasis tends to be thicker and scalier, while lichen planus is often flatter and purplish.)
- Journey Through Time: Both conditions can be chronic, meaning they can come and go over time, with periods of remission and flare-ups.
- Genetic Threads: Both have a genetic component, though the specific genes involved differ. This means family history can play a role in both.
- Immune Spotlight: Both are linked to an overactive immune system, leading to inflammation and the characteristic skin lesions.
- Beyond the Surface: Both can affect other areas beyond the skin, including nails, scalp, and even joints in some cases.
Remember, while shared threads connect them, psoriasis and lichen planus remain distinct entities. Understanding their similarities, however, can provide a broader perspective, promote empathy, and pave the way for more effective management and support for individuals battling either condition.
| Check out More Articles | |
| Difference Between Thick and Thin Skin Anatomy | |
| Difference Between Enzyme and Coenzyme | |
| Difference Between Infection and Infestation | |