Pemphigus Vulgaris Vs Bullous Pemphigoid: Dermatological conditions often present a complex landscape, and among them, Pemphigus Vulgaris and Bullous Pemphigoid stand out as autoimmune blistering disorders. While they share certain similarities, their clinical features, underlying mechanisms, and target antigens set them apart. Understanding the differences between Pemphigus Vulgaris and Bullous Pemphigoid is crucial for accurate diagnosis and tailored treatment approaches.
Pemphigus Vulgaris Vs Bullous Pemphigoid
Here's a table summarizing the key differences between Pemphigus Vulgaris and Bullous Pemphigoid:
|
Feature |
Pemphigus Vulgaris |
Bullous Pemphigoid |
|
Epidemiology |
Typically middle-aged individuals, with a peak incidence in the fifth and sixth decades of life. |
More common in the elderly, often affecting individuals over the age of 60. |
|
Clinical Presentation |
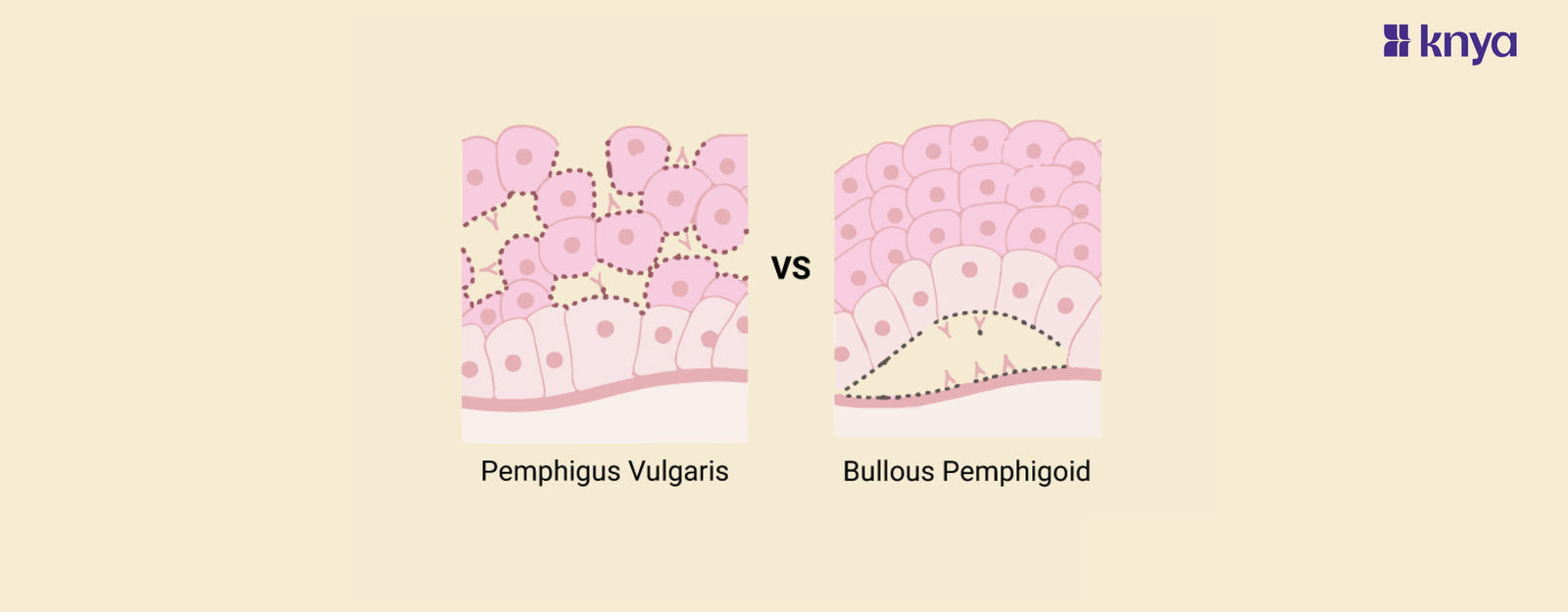
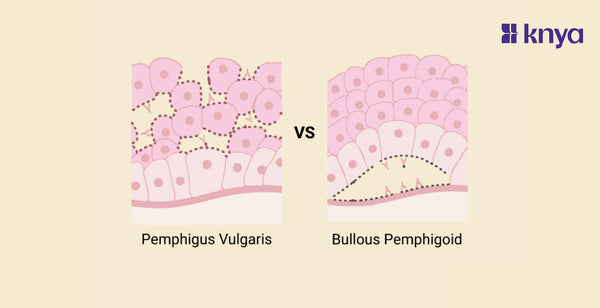
Intraepithelial blistering, fragile blisters that easily rupture, leading to erosions on the skin and mucous membranes. |
Subepidermal blisters, tense and intact bullae, often localized to flexural areas. |
|
Target Antigens |
Autoantibodies target desmogleins, specifically desmoglein-3 and desmoglein-1, components of desmosomes. |
Autoantibodies primarily target hemidesmosomal proteins, particularly BP180 (collagen XVII) and BP230. |
|
Histopathology |
Suprabasal acantholysis, presence of Tzanck cells in biopsy reflecting the destruction of epidermal cells. |
Subepidermal blistering with an inflammatory infiltrate, often eosinophilic, and sometimes neutrophilic. |
|
Mucous Membrane Involvement |
Frequently involves mucous membranes, leading to painful erosions in the oral cavity and other mucosal surfaces. |
Mucous membrane involvement is less common, and oral lesions, if present, are generally milder. |
|
Treatment Approach |
High-dose systemic corticosteroids, often combined with immunosuppressive agents. |
Systemic corticosteroids, usually at lower doses. Immunomodulatory drugs may be used as well. |
What is Pemphigus Vulgaris?
Pemphigus Vulgaris is a rare autoimmune blistering disorder characterized by the development of intraepithelial blisters, erosions, and ulcerations on the skin and mucous membranes. This condition is caused by the production of autoantibodies, specifically IgG antibodies, that target desmosomal proteins, particularly desmoglein-3 and desmoglein-1. Desmosomes are adhesive structures that play a crucial role in maintaining the integrity of epithelial cells.
Key Features of Pemphigus Vulgaris:
- Blister Formation: Autoantibodies target desmogleins, leading to the breakdown of desmosomes and causing separation between epidermal cells. This results in the formation of fragile blisters.
- Mucous Membrane Involvement: Pemphigus Vulgaris often involves mucous membranes, leading to painful erosions in the oral cavity, throat, and other mucosal surfaces.
- Nikolsky's Sign: A characteristic clinical sign where slight rubbing of the skin adjacent to a blister results in the formation of new blisters, indicating the fragility of the skin.
- Age of Onset: It typically occurs in middle-aged individuals, with a peak incidence in the fifth and sixth decades of life.
- Association with Other Conditions: Pemphigus Vulgaris may be associated with other autoimmune conditions, such as myasthenia gravis or thymoma.
- Treatment: Management involves high-dose systemic corticosteroids to suppress the autoimmune response, often combined with immunosuppressive agents. Long-term treatment and monitoring are usually necessary.
Pemphigus Vulgaris can have a severe and chronic course, with potential complications and a risk of mortality if not effectively managed. Early diagnosis and appropriate treatment are crucial in improving outcomes for individuals with this autoimmune blistering disorder.
What is Bullous Pemphigoid?
Bullous Pemphigoid is another autoimmune blistering disorder characterized by the development of tense, subepidermal blisters on the skin. Unlike Pemphigus Vulgaris, Bullous Pemphigoid involves the formation of blisters beneath the epidermal basement membrane. The condition is primarily associated with autoantibodies targeting hemidesmosomal proteins, particularly BP180 (collagen XVII) and BP230.
Key Features of Bullous Pemphigoid:
- Blisters and Bullae: Bullous Pemphigoid results in the formation of large, tense bullae (fluid-filled blisters) on the skin. These bullae are often intact and do not rupture easily.
- Age of Onset: Bullous Pemphigoid is more common in the elderly population, often affecting individuals over the age of 60.
- Lesion Distribution: There is a predilection for flexural areas, such as the groin, axillae, and abdominal folds. Lesions may also occur on other parts of the body.
- Mucous Membrane Involvement: Mucous membrane involvement is less common compared to Pemphigus Vulgaris, and oral lesions, if present, are generally milder.
- Histopathology: Biopsy shows subepidermal blistering with an inflammatory infiltrate, often eosinophilic and sometimes neutrophilic.
- Nikolsky's Sign: Unlike Pemphigus Vulgaris, Bullous Pemphigoid typically exhibits a negative Nikolsky's sign, where rubbing of the skin does not result in blister formation.
- Treatment: Treatment involves systemic corticosteroids, usually at lower doses than those used for Pemphigus Vulgaris. Immunomodulatory drugs may also be employed. Relapses are common, and long-term management is often needed.
Bullous Pemphigoid generally has a better prognosis compared to Pemphigus Vulgaris, and mortality is lower. However, the chronic nature of the disease requires ongoing medical management to control symptoms and prevent relapses. Early diagnosis and appropriate treatment are essential for improving the quality of life for individuals with Bullous Pemphigoid.
Similarity Between Pemphigus Vulgaris and Bullous Pemphigoid
Similarities Between Pemphigus Vulgaris and Bullous Pemphigoid:
- Autoimmune Nature:
- Both Pemphigus Vulgaris and Bullous Pemphigoid are autoimmune blistering disorders characterized by the production of autoantibodies that target components of the skin.
- Skin Blistering:
- Both conditions lead to the formation of blisters on the skin, though the location and characteristics of these blisters differ.
- Immunoglobulin G (IgG) Antibodies:
- The predominant class of autoantibodies in both disorders is IgG, specifically targeting proteins involved in maintaining the integrity of the skin.
- Chronic Course:
- Both conditions can have a chronic course, requiring long-term management to control symptoms and prevent relapses.
- Potential for Mucous Membrane Involvement:
- While mucous membrane involvement is more common in Pemphigus Vulgaris, both disorders have the potential to affect mucous membranes, leading to erosions and blistering.
- Inflammatory Infiltrate:
- Histopathological examination of biopsied tissue from both disorders reveals an inflammatory infiltrate in the affected areas.
- Systemic Treatment:
- Systemic corticosteroids and immunosuppressive agents are common components of the treatment strategy for both Pemphigus Vulgaris and Bullous Pemphigoid.
While these similarities exist, it's crucial to recognize the distinct features and differences between Pemphigus Vulgaris and Bullous Pemphigoid to ensure accurate diagnosis and appropriate treatment approaches.
|
Check out More Articles |
|