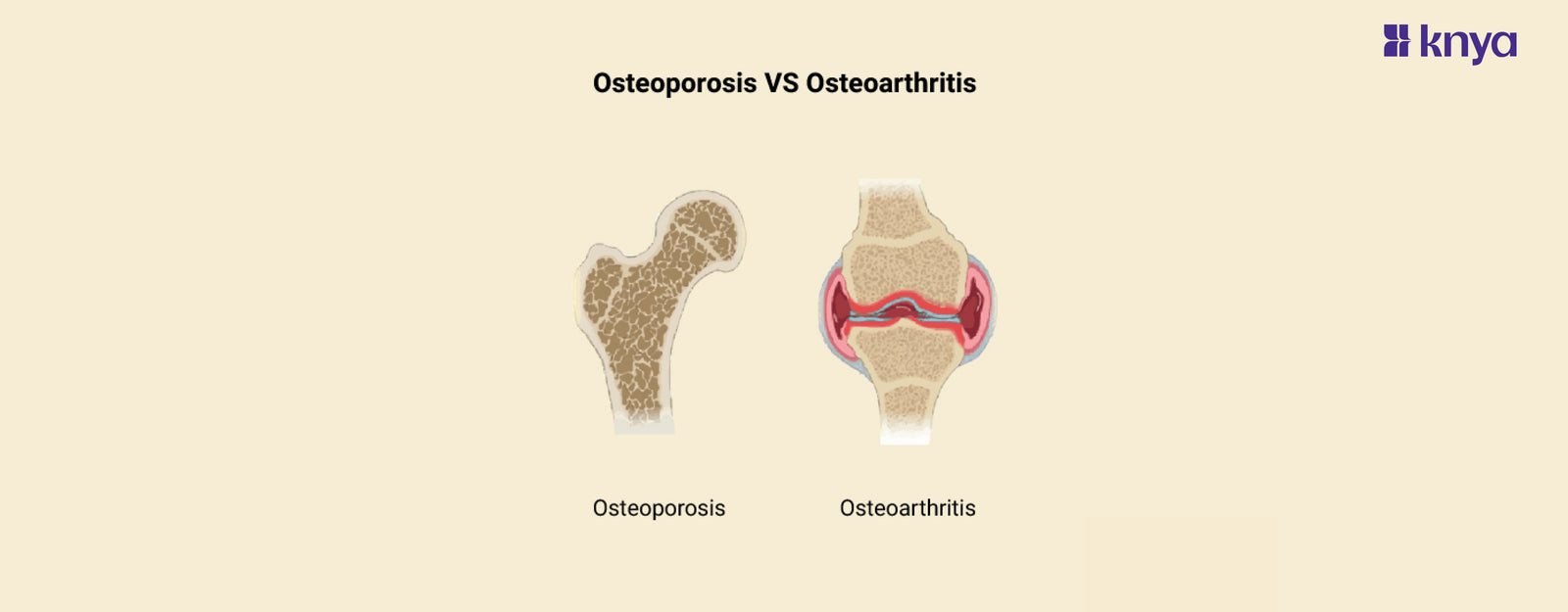
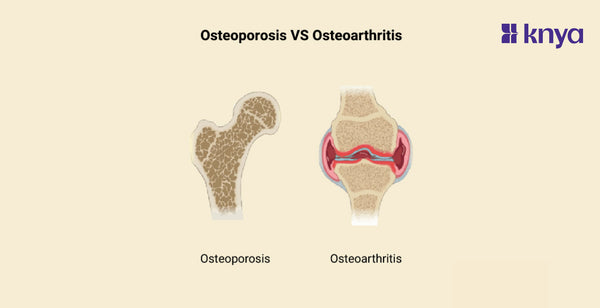
Difference Between Osteoporosis and Osteoarthritis: Osteoporosis and Osteoarthritis, though both involving bones, are distinctly different conditions. Osteoporosis, often called the "silent thief," weakens bones from within, increasing fracture risk, typically without initial pain. Osteoarthritis, on the other hand, affects the joints themselves, causing stiffness, pain, and reduced mobility due to cartilage wear and tear. While the "osteo" in their names hints at a bone connection, Osteoporosis vs Osteoarthritis highlights their unique targets and symptoms, demanding different treatment approaches.
Osteoporosis
- Bone disease: Weakening of bones, increasing fracture risk.
- Silent thief: Often progresses without symptoms until a fracture.
- Risk factors: Age, female sex, menopause, low calcium/vitamin D, inactivity.
- Prevention: Calcium, vitamin D, weight-bearing exercise, medication.
Osteoarthritis
- Joint disease: Wear-and-tear breakdown of cartilage in joints.
- Pain and stiffness: Affects hands, hips, knees, spine, neck.
- Risk factors: Age, joint injury, obesity, overuse.
- Management: Pain relief, physical therapy, joint replacement, injections.
Differences Between Osteoporosis and Osteoarthritis
Osteoporosis and osteoarthritis are both conditions related to the bones and joints, but they affect the body in different ways. Here's an overview of each condition and then the differences between arterial osteoporosis and osteoarthritis:
|
Aspect |
Arterial Osteoporosis |
Osteoarthritis |
|
Nature of Condition |
Affects bone density and strength, particularly in arteries. |
Affects the cartilage in joints, leading to joint degeneration. |
|
Location |
Primarily affects arterial walls. |
Affects weight-bearing joints like knees, hips, spine, as well as hands and fingers. |
|
Primary Symptom |
May manifest as arterial stiffness and calcification. |
Joint pain, stiffness, and inflammation are common symptoms. |
|
Diagnostic Techniques |
Diagnosis involves imaging techniques to assess arterial health. |
Diagnosis involves physical examination, X-rays, and other imaging studies of affected joints. |
|
Risk Factors |
Factors may include age, genetics, hormonal changes, and lifestyle factors like diet and exercise. |
Risk factors include age, obesity, joint injury, and genetics. |
|
Treatment Approaches |
Treatment may involve lifestyle modifications, medications to improve arterial health, and managing underlying conditions. |
Treatment may include pain management, physical therapy, medications, and surgery in severe cases. |
|
Complications |
Complications may include increased risk of cardiovascular events like heart attacks and strokes. |
Complications may include joint deformity, limited mobility, and decreased quality of life. |
|
Prevention Strategies |
Focus on maintaining cardiovascular health through lifestyle changes. |
Focus on weight management, joint protection techniques, and muscle strengthening exercises. |
|
Diagnostic Tools |
Relies on imaging techniques like ultrasound, CT scans, or MRI to assess arterial health. |
Utilizes physical examination, X-rays, and MRI scans to assess joint health. |
|
Primary Manifestation |
Manifests primarily in the cardiovascular system. |
Manifests primarily in the joints, causing pain and stiffness. |
Browse Best Scrubs Collection
What is Osteoporosis?
Osteoporosis is a bone disease that causes weaker and brittle bones owing to low bone mass and density. It is popularly known as the "silent thief" since it causes no symptoms until a fracture occurs. It mostly affects the spine, hips, and wrists. Risk factors include age, gender, ethnicity, family history, certain drugs, and lifestyle choices such as smoking and inadequate calcium consumption. The treatment focuses on preventing fractures by medication, exercise, and dietary modifications.
Key Features of Osteoporosis:
- The defining trait is low bone density and mass, which makes bones fragile and brittle and prone to fractures.
- It mostly impacts bone growth and breakdown balance. Bone is continually remodelled, but in osteoporosis, breakdown exceeds creation.
- Often unnoticed until a fracture occurs, resulting in acute pain, incapacity, and an increased risk of future fractures.
- Risk factors include age, ethnicity, family history, hormonal changes (e.g., menopause), certain drugs, dietary deficiencies (calcium, vitamin D), and inactivity.
Explore All Women's Scrub
What is Osteoarthritis?
Osteoarthritis is the most prevalent kind of arthritis, impacting millions globally. The deterioration of cartilage, the protective cushion in joints, causes discomfort, stiffness, and limited mobility. It often affects weight-bearing joints such as the knees, hips, and hands and is frequently associated with age and risk factors such as obesity, past injuries, and joint abuse. While there is no cure, treatment includes pain medication, physical therapy, and joint injections to enhance function and quality of life.
Key Features of Osteoarthritis:
- It affects the cartilage that cushions the joints, causing wear and tear, inflammation, and discomfort.
- The breakdown of cartilage is caused by a variety of causes such as ageing, injury, obesity, and mechanical stress on joints.
- Symptoms consist of joint discomfort, stiffness, edoema, and limited range of motion, which generally increase with exercise.
- Risk factors include age, joint injuries, obesity, heredity, recurrent joint stress, and underlying illnesses such as rheumatoid arthritis.
Shop Best Lab Coats from Here!
Similarities Between Osteoporosis and Osteoarthritis
- Both osteoporosis and osteoarthritis are age-related illnesses.
- Both can result in diminished mobility and quality of life.
- Diet and exercise are two lifestyle factors that can impact how both illnesses evolve.
- Both may benefit from early detection and treatment efforts to avoid consequences.
- Osteoporosis and osteoarthritis may be genetically predisposed.
While the word "osteo" indicates bone involvement, osteoporosis and osteoarthritis are separate illnesses that require different therapies. Osteoporosis weakens the bone's structure, making it brittle and prone to fractures; it frequently progresses silently until a break occurs. Osteoarthritis, on the other hand, assaults the joints, causing pain, stiffness, and limited mobility as the cartilage cushioning the bones wears away. Understanding the basic differences between osteoporosis and osteoarthritis enables people to seek proper diagnosis, treatment, and preventative measures to keep their bones and joints healthy throughout their lifetimes.
Order the Best Jogger Scrub from Here!
| Check out More Articles | |
| Difference Between Cartilage and Bone | |
| Difference Between Endocrine and Exocrine Glands | |
| Difference Between Cell Wall and Cell Membrane | |