Leukoplakia Vs Lichen Planus: Oral health encompasses a myriad of conditions, and among them, leukoplakia and lichen planus stand out as distinctive entities, each presenting unique challenges and characteristics. Both conditions affect the mucous membranes within the oral cavity, but their origins, appearance, and potential implications diverge. Understanding the differences between leukoplakia and lichen planus is vital for accurate diagnosis, appropriate management, and ensuring optimal oral health.
Leukoplakia Vs Lichen Planus
Here's a table outlining the key differences between leukoplakia and lichen planus:
|
Feature |
Leukoplakia |
Lichen Planus |
|
Definition |
White, thickened patches on oral mucosa, potentially precancerous |
Inflammatory condition with white, lacy patches or sores on mucous membranes |
|
Appearance |
Irregular white patches, varying texture (smooth, rough, nodular) |
White, reticular (lace-like) patterns or erosive sores |
|
Cause |
Chronic irritation, tobacco use, alcohol consumption |
Immune system response, potential triggers include medications, hepatitis C, autoimmune factors |
|
Location |
Tongue, inside cheeks, gums |
Inside of cheeks, tongue, other mucous membranes |
|
Symptoms |
Usually asymptomatic; may have sensitivity or discomfort |
May cause discomfort, burning sensations, pain in erosive forms |
|
Risk of Malignancy |
Some types have higher potential for malignancy; biopsy may be recommended |
Generally considered benign; certain forms may slightly elevate oral cancer risk |
|
Biopsy Recommendation |
Biopsy often recommended for accurate diagnosis and management |
Biopsy may be performed for diagnosis, especially if erosive or suspected of dysplasia |
|
Treatment Approach |
Removal of source of irritation, monitoring for changes |
Symptomatic relief; topical or systemic corticosteroids for severe cases |
|
Prognosis |
Variable; may depend on underlying causes and potential for malignancy |
Generally good; most cases do not progress to malignancy |
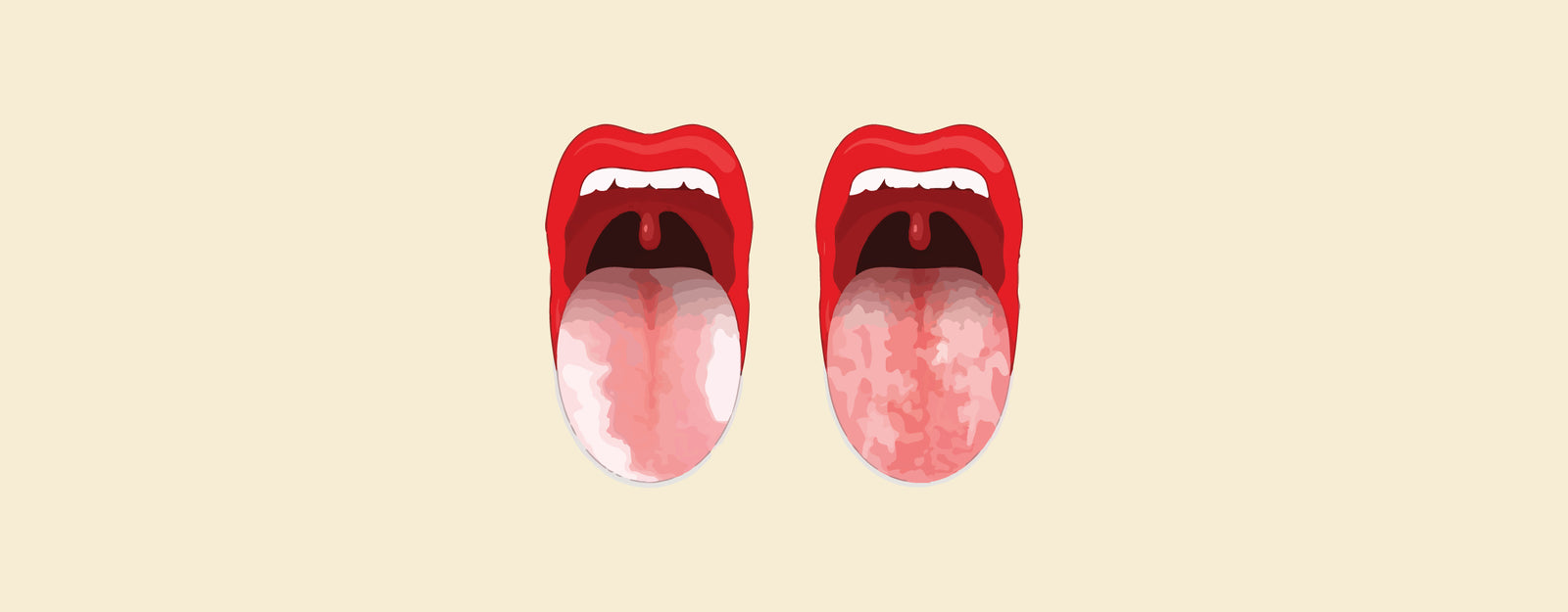
What is Leukoplakia?
Leukoplakia is a condition characterized by the development of white or grayish patches on the mucous membranes of the mouth and sometimes the genital area. These patches can occur on the tongue, inside of the cheeks, gums, or the floor of the mouth. While leukoplakia is generally considered a benign condition, some forms may carry a risk of becoming precancerous.
Key features of leukoplakia include:
- Appearance: The patches associated with leukoplakia are often white or gray and may have irregular borders. The texture can vary, ranging from smooth to rough or nodular.
- Cause: The exact cause of leukoplakia is not always clear, but it is often associated with chronic irritation, such as tobacco use, alcohol consumption, or other forms of local irritation in the oral cavity.
- Symptoms: In many cases, leukoplakia is asymptomatic and does not cause pain or discomfort. However, some individuals may experience sensitivity or irritation in the affected areas.
- Risk of Malignancy: While most cases of leukoplakia are benign, certain types have a higher potential for becoming precancerous or cancerous. A biopsy may be recommended to assess the degree of dysplasia and guide further management.
- Diagnosis: Diagnosis is typically based on clinical examination, and a biopsy may be performed to determine the nature of the lesion and assess the risk of malignancy.
- Treatment: Treatment for leukoplakia often involves removing or addressing the source of irritation, such as quitting smoking or reducing alcohol consumption. Regular monitoring is essential, and in cases with a higher risk of malignancy, more aggressive interventions may be recommended.
Cause of Leukoplakia
The exact cause of leukoplakia is not always clear-cut, and it can arise from various factors. However, the condition is often associated with chronic irritation or damage to the mucous membranes, particularly in the oral cavity. The primary causes and risk factors for leukoplakia include:
- Tobacco Use:
- Smoking tobacco (cigarettes, cigars, pipes) is a significant risk factor for leukoplakia. The chemicals in tobacco smoke can irritate and damage the mucous membranes in the mouth.
- Smokeless Tobacco:
- Chewing tobacco or using snuff (smokeless tobacco) is also strongly associated with leukoplakia. Direct contact of these products with the oral tissues can lead to irritation and the development of white patches.
- Alcohol Consumption:
- Excessive and chronic alcohol consumption is another common risk factor for leukoplakia. Alcohol can contribute to mucosal irritation and inflammation.
- Combined Use of Tobacco and Alcohol:
- The risk of developing leukoplakia increases significantly when there is a combination of tobacco and alcohol use. This combination has a synergistic effect on mucosal irritation and damage.
- Oral Hygiene Factors:
- Poor oral hygiene, including irregular dental care and the presence of dental appliances that cause chronic irritation, may contribute to the development of leukoplakia.
- Nutritional Deficiencies:
- Some studies suggest that deficiencies in certain nutrients, such as vitamin A, may play a role in the development of leukoplakia.
- Chronic Mechanical Irritation:
- Long-term irritation from rough teeth, dentures, or other oral appliances can contribute to leukoplakia
Symptoms of Leukoplakia
Leukoplakia is a condition characterized by the development of thickened, white or gray patches in the mouth, particularly on the tongue, gums, or insides of the cheeks. While these patches are usually painless, they can sometimes indicate underlying issues. Here are the common symptoms associated with leukoplakia:
- White or Gray Patches: The primary and most noticeable symptom is the presence of white or gray patches in the mouth. These patches may have irregular borders and can vary in size.
- Thickened or Raised Areas: The affected areas may feel thicker or raised compared to the surrounding normal tissue.
- Texture Changes: The texture of the patches may differ from the surrounding oral tissues. They can feel rough or scaly.
- Persistent Lesions: Unlike common oral irritations that resolve on their own, leukoplakic patches tend to persist and may not go away over time.
- Localized Irritation: Some individuals may experience localized irritation or discomfort in the areas where leukoplakic patches are present, especially if there is friction or pressure.
- Increased Sensitivity: In some cases, the patches may become sensitive to touch, heat, or spicy foods.
- Risk of Dysplasia: While not a symptom that can be directly felt, leukoplakia carries the risk of dysplasia (abnormal cell changes), which is a concern because it can progress to oral cancer.
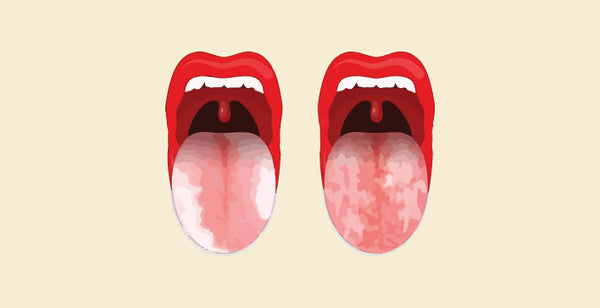
What is Lichen Planus
Lichen planus is an inflammatory skin and mucous membrane condition that can affect various parts of the body. The exact cause of lichen planus is not fully understood, but it is believed to involve an abnormal immune response. Here are key aspects of lichen planus:
- Appearance:
- In the skin, lichen planus typically presents as flat-topped, purple, or white lesions that may have a lacy or net-like pattern.
- In mucous membranes, such as the mouth (oral lichen planus), lesions can appear as white, lacy patches, or as red, swollen areas.
- Location:
- Lichen planus can occur on the skin, mucous membranes (oral, genital, esophageal), nails, and scalp.
- The oral cavity is a common site for lichen planus, with lesions appearing on the insides of the cheeks, tongue, and gums.
- Symptoms:
- Itching is a common symptom, especially in skin involvement.
- In oral lichen planus, patients may experience soreness, a burning sensation, or discomfort in the affected areas.
- Diagnosis:
- Diagnosis is often based on clinical examination, considering the characteristic appearance of the lesions.
- In some cases, a biopsy may be performed to confirm the diagnosis and rule out other conditions.
- Triggers:
- Lichen planus can be triggered by various factors, including stress, certain medications (like beta-blockers or non-steroidal anti-inflammatory drugs), infections, and sometimes, contact with certain chemicals.
- Duration:
- Lichen planus can be a self-limiting condition, meaning it may resolve on its own without treatment.
- However, in some cases, it may persist for a longer duration, requiring medical management.
- Treatment:
- Treatment aims to alleviate symptoms and may include topical or oral corticosteroids, antihistamines, or other medications depending on the severity and location of the lesions.
- Regular monitoring and follow-up with a dermatologist or other healthcare professionals are often recommended.
It's important to note that while lichen planus can cause discomfort, it is not contagious, and it does not increase the risk of cancer. If you suspect you have lichen planus or experience persistent skin or mucosal changes, it is advisable to seek medical attention for an accurate diagnosis and appropriate management.
Shop best Lab Coats from Here!
Cause of Lichen Planus
The exact cause of lichen planus is not fully understood, and it is considered to be a complex autoimmune-related condition. Lichen planus occurs when the immune system attacks the cells of the skin or mucous membranes, leading to inflammation and the characteristic symptoms associated with the condition. While the precise triggers remain unclear, several factors are believed to contribute to the development of lichen planus:
- Autoimmune Reaction:
- Lichen planus is thought to result from an abnormal immune response in which the body's immune system mistakenly targets its own cells. The reasons for this autoimmune reaction are not well-defined.
- Genetic Predisposition:
- There may be a genetic predisposition to lichen planus, as it sometimes appears to run in families. However, a clear genetic link has not been established.
- Inflammatory Disorders:
- Individuals with other inflammatory conditions, such as rheumatoid arthritis, may have an increased risk of developing lichen planus. The exact relationship between lichen planus and these disorders is not fully understood.
- Viral Infections:
- Some studies suggest a potential link between certain viral infections and the development of lichen planus. Viruses such as hepatitis C have been associated with an increased risk of lichen planus.
- Medications:
- Certain medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), beta-blockers, and antimalarial drugs, have been implicated as potential triggers for lichen planus in some individuals.
- Stress:
- While not a direct cause, stress and emotional factors may exacerbate lichen planus symptoms. Stress management techniques may be beneficial in managing the condition.
Symptoms of Lichen Planus
Lichen planus is an inflammatory condition that can affect the skin, mucous membranes, and nails. The symptoms of lichen planus can vary depending on the specific area of the body affected. Here are the common symptoms associated with lichen planus:
- Skin Involvement:
- Flat-topped, purple or white lesions on the skin with a lacy or net-like pattern.
- Itching, which can be intense, especially in the affected areas.
- Oral (Mouth) Involvement (Oral Lichen Planus):
- White, lacy patches or red, swollen areas in the mouth, particularly on the insides of the cheeks, tongue, or gums.
- Soreness, a burning sensation, or discomfort in the oral cavity.
- Difficulty eating or drinking, especially if the lesions are painful.
- Genital Involvement (Genital Lichen Planus):
- Itching and discomfort in the genital area.
- White, shiny, or red patches on the genitals.
- Painful intercourse in some cases.
- Nail Involvement:
- Grooves or ridges on the nails.
- Pitting (small dents or depressions) on the nail surface.
- Nail thinning or splitting.
- Scalp Involvement:
- Redness, scaling, or patchy hair loss on the scalp.
- Esophageal Involvement (Esophageal Lichen Planus):
- Rarely, lichen planus can affect the esophagus, leading to difficulty swallowing or discomfort.
- General Symptoms:
- Lichen planus may be associated with stress, and emotional or physical trauma can sometimes trigger or worsen the condition.
Similarity Between Leukoplakia Vs Lichen Planus
Leukoplakia and lichen planus are both conditions that affect the mucous membranes, particularly in the oral cavity, and they share some similarities:
- Appearance:
- Both leukoplakia and lichen planus can present as white patches or lesions on the mucous membranes. The patches may have a whitish or grayish color, and their appearance can vary in texture.
- Oral Cavity Involvement:
- Both conditions commonly affect the oral cavity. Leukoplakia may occur on the tongue, inside the cheeks, or on the gums. Lichen planus often involves the inside of the cheeks, tongue, and other mucous membranes in the mouth.
- Potential for Precancerous Changes:
- In some cases, leukoplakia lesions may be precancerous, and there is an increased risk of malignant transformation. While lichen planus is generally considered a benign condition, certain forms may slightly elevate the risk of oral cancer.
- Need for Professional Evaluation:
- Both leukoplakia and lichen planus require professional evaluation for an accurate diagnosis and appropriate management. Biopsy and microscopic examination may be recommended to determine the nature of the lesions and assess the risk of malignancy.
- Risk Factors:
- Tobacco use, both smoking and smokeless forms, is a common risk factor for both leukoplakia and lichen planus. Alcohol consumption is another shared risk factor.
- Association with Chronic Irritation:
- Chronic irritation is often associated with both conditions. Leukoplakia may result from chronic irritation due to tobacco or alcohol use, while lichen planus may be linked to inflammatory responses triggered by various factors.
Despite these similarities, it's crucial to note that leukoplakia and lichen planus are distinct conditions with different underlying causes, risk profiles, and potential outcomes. The management and treatment approaches for each condition can also differ based on their specific characteristics and associated risks. Therefore, a thorough evaluation by a healthcare professional is essential for an accurate diagnosis and appropriate care.
|
Check out More Articles |
|