Difference Between In-Stent Restenosis and Stent Thrombosis: In-stent restenosis and stent thrombosis are two different consequences of coronary stent implantation. As a result of tissue growth inside the stent, in-stent restenosis causes the treated artery to re-narrow. This condition usually results in repeated symptoms over time. On the other hand, stent thrombosis is distinguished by the abrupt aggregation of a thrombus inside the stent, which may result in acute vascular blockage and myocardial infarction. Even though both need immediate attention, a proper diagnosis and management plan depend on a knowledge of their distinct processes and clinical manifestations.
Difference between Stent Restenosis and Stent Thrombosis
In-Stent Restenosis (ISR) is the slow constriction of a previously stented artery due to tissue proliferation within the stent, resulting in symptoms such as recurring chest discomfort. On the other hand, Stent Thrombosis is defined by the abrupt and severe formation of a blood clot inside or close to the stent, which can result in myocardial infarction and other potentially fatal consequences. The table below provides the differences between Stent Restenosis and Stent Thrombosis.
|
Aspect |
In-Stent Restenosis |
Stent Thrombosis |
|
Definition |
Gradual re-narrowing of a previously stented artery segment due to tissue proliferation within the stent. |
Acute formation of a blood clot within or adjacent to the stent, leading to sudden occlusion of the coronary artery. |
|
Pathophysiology |
Tissue proliferation, including smooth muscle cell growth or scar tissue formation, within the stent. |
Formation of a blood clot (thrombus) within or near the stent, often triggered by factors like incomplete stent apposition or discontinuation of antiplatelet medications. |
|
Onset |
Develops gradually over time. |
Occurs acutely. |
|
Clinical Presentation |
Recurrent chest pain (angina), signs of reduced blood flow to the heart muscle. |
Sudden onset of severe chest pain, shortness of breath, signs of myocardial infarction or cardiac arrest. |
|
Diagnostic Evaluation |
Stress tests, coronary angiography, non-invasive imaging (e.g., CT angiography, MRI). |
Clinical presentation, electrocardiogram (ECG) changes, confirmation via coronary angiography. |
|
Treatment Options |
Medication adjustments, PCI (balloon angioplasty, drug-coated balloons), coronary artery bypass grafting (CABG). |
Immediate administration of antiplatelet medications (e.g., aspirin, P2Y12 inhibitors), anticoagulants (e.g., heparin), emergency PCI with thrombus aspiration or balloon angioplasty, CABG in severe cases. |
|
Prognosis |
Generally not life-threatening but can impact quality of life. |
Can lead to myocardial infarction, cardiac arrest, or death if not promptly treated. |
|
Preventive Measures |
Medication adherence, lifestyle modifications (e.g., healthy diet, exercise), regular follow-up with healthcare providers. |
Continuation of antiplatelet therapy as prescribed, avoidance of known triggers (e.g., abrupt discontinuation of antiplatelet medications). |
Browse The Best Scrubs Collection!
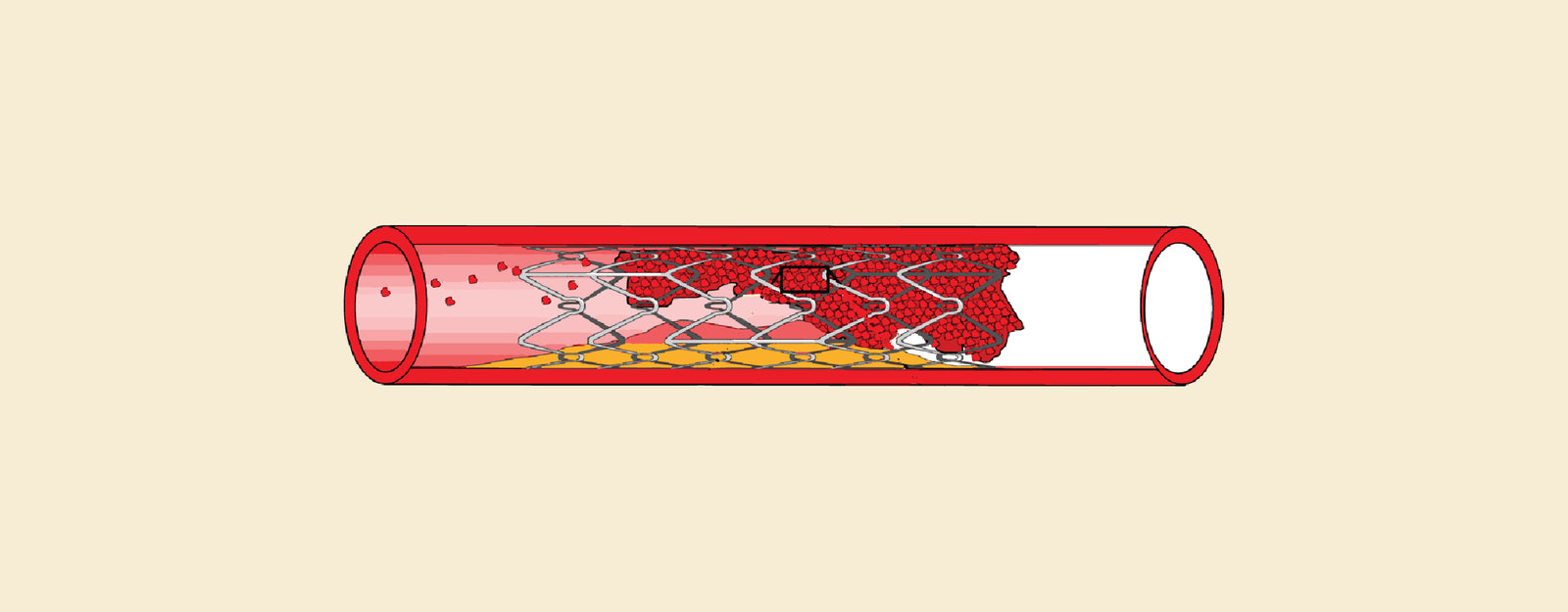
What is In-Stent Restenosis?
In-Stent Restenosis (ISR) is the slow re-narrowing of a previously treated coronary artery section with a stent. The development of tissue, such as smooth muscle cells or scar tissue, inside the stent is the cause of this re-narrowing. ISR can cause symptoms like angina, persistent chest discomfort, or show signs of decreased blood flow to the heart muscle. To reopen the narrowed arterial segment and provide the heart with enough blood flow, it usually grows gradually over time and may need additional treatments, such as medication modifications, balloon angioplasty, or repeat stent implantation.
Causes of In-Stent Restenosis
- Neointimal Hyperplasia: The most frequent reason for ISR is this condition. It involves the growth of smooth muscle cells inside the stent, which causes an overabundance of tissue to develop and constrict the artery.
- Inflammatory Response: The implantation of a stent may cause the artery wall to become inflamed, which might result in the creation of scar tissue surrounding the stent and worsen restenosis.
- Stent Material and Design: Some stent materials or designs may raise the likelihood of tissue proliferation or stimulate a stronger inflammatory response, which can put a patient at risk for ISR.
- Stent Underexpansion: If the stent is not sufficiently expanded during the initial installation process, parts of the diseased artery segment may remain uncovered, making them vulnerable to restenosis.
- Incomplete Revascularization: ISR in untreated areas may arise from the first procedure's inadequate treatment of all diseased coronary artery segments.
Symptoms of In-Stent Restenosis
- Recurrent Chest Pain (Angina): Individuals with ISR may feel pain or discomfort in their chests that is comparable to what they experienced when they had angina. Stress or physical exertion can cause this chest pain, which can be eased by resting or taking medicine.
- Breathlessness: ISR-related reduced blood flow to the heart muscle can result in insufficient oxygen delivery, which can cause dyspnea, particularly during physical activity or activities that elevate the heart's workload.
- Fatigue: Especially during physical exertion, an ISR-related decrease in blood flow to the heart muscle may cause fatigue or a generalized feeling of weakness.
- Exercise Intolerance: Individuals with ISR may discover that, as a result of insufficient blood flow to the heart, they are unable to tolerate the same degree of physical activity as before or that they tire out quickly when exercising.
- Palpitations: If the heart is trying harder to make up for decreased blood flow, some people with ISR may suffer palpitations, irregular heartbeats, or feelings of their heart racing or hammering.
What is Stent Thrombosis?
Stent Thrombosis is a serious complication that occurs after inserting a stent into a restricted artery, most commonly during coronary angioplasty. It involves the development of a blood clot inside the stent, which can severely impair blood flow to the heart and other essential organs and cause a heart attack or stroke. Stent Thrombosis is a medical emergency that can happen soon after the procedure (acute), during the first month (subacute), or later (late). Strict adherence to antiplatelet drugs and modifying one's lifestyle to reduce risk factors like smoking and high cholesterol are examples of preventive strategies.
Causes of Stent Thrombosis
- Incomplete Endothelialization: The endothelium, which lines the inside of the blood vessel, might not completely enclose the stent struts following stent implantation. This insufficient covering may cause clots to develop.
- Stent Malapposition: When a stent is improperly positioned on the vascular wall, it can cause turbulent blood flow, which raises the possibility of clot development.
- Stent Underexpansion: Blood flow may be impeded in certain parts of the stent if it is not sufficiently expanded to the appropriate diameter, which could encourage the formation of clots.
- Stent Type and Design: Different stent designs may have varying thrombosis risks. In comparison to bare-metal stents (BMS), drug-eluting stents (DES) have a somewhat increased risk of late stent thrombosis; however, because of decreased restenosis, DES have a lower overall incidence of thrombosis.
- Underlying Patient Factors: Endothelial dysfunction and an elevated risk of clotting can be exacerbated by diseases such as diabetes, hyperlipidemia, hypertension, and smoking.
- Acute Coronary Syndrome (ACS): Because of the prothrombotic state linked to ACS circumstances, patients with unstable angina or myocardial infarction are more likely to experience Stent Thrombosis.
Symptoms of Stent Thrombosis
- Chest Pain or Discomfort: This is the most common symptom. It could cause a heaviness, tightness, pinching, or pressing sensation in the chest. Radiation pain to the arms, jaw, back, or abdomen is possible.
- Breathlessness: The inability to breathe or the sensation that you are not breathing enough, particularly when you are resting or exerting yourself very little.
- Palpitations: Palpitations are the feeling of a fast, thumping, or racing heartbeat.
- Sweating: Severe perspiration that frequently comes with clamminess.
- Vomiting or Nausea: Certain people may feel queasy, throw up, or have indigestion.
- Weakness or Fatigue: Feeling abnormally weak or exhausted, even after moderate exercise.
- Dizziness or Lightheadedness: This feeling, which may be accompanied by chest pain, is that of being faint, dizzy, or lightheaded.
Shop Best Lab Coats From Here!
Similarities Between Stent Restenosis and Stent Thrombosis
- Clinical Presentation: It might be difficult to distinguish between the two because they can both present with symptoms that are similar to acute coronary syndrome.
- Timing: They can happen at different times following the implantation of a stent; restenosis usually happens months or years later, whereas thrombosis can happen acutely, subacutely, or later.
- Connection to Stenting: The two issues are caused directly by the stent's placement in the artery.
- Risk Factors: Age, smoking, diabetes, and other conditions raise the chance of both problems.
- Diagnostic Evaluation: Coronary angiography, frequently combined with intravascular imaging, may be necessary for both to be evaluated.
Order the Best Jogger Scrub From Here!
| Check out More Articles | |
| Difference Between Tendon and Ligament | |
| Difference Between Seizure and Epilepsy | |
| Difference Between Hypothyroidism and Hyperthyroidism | |