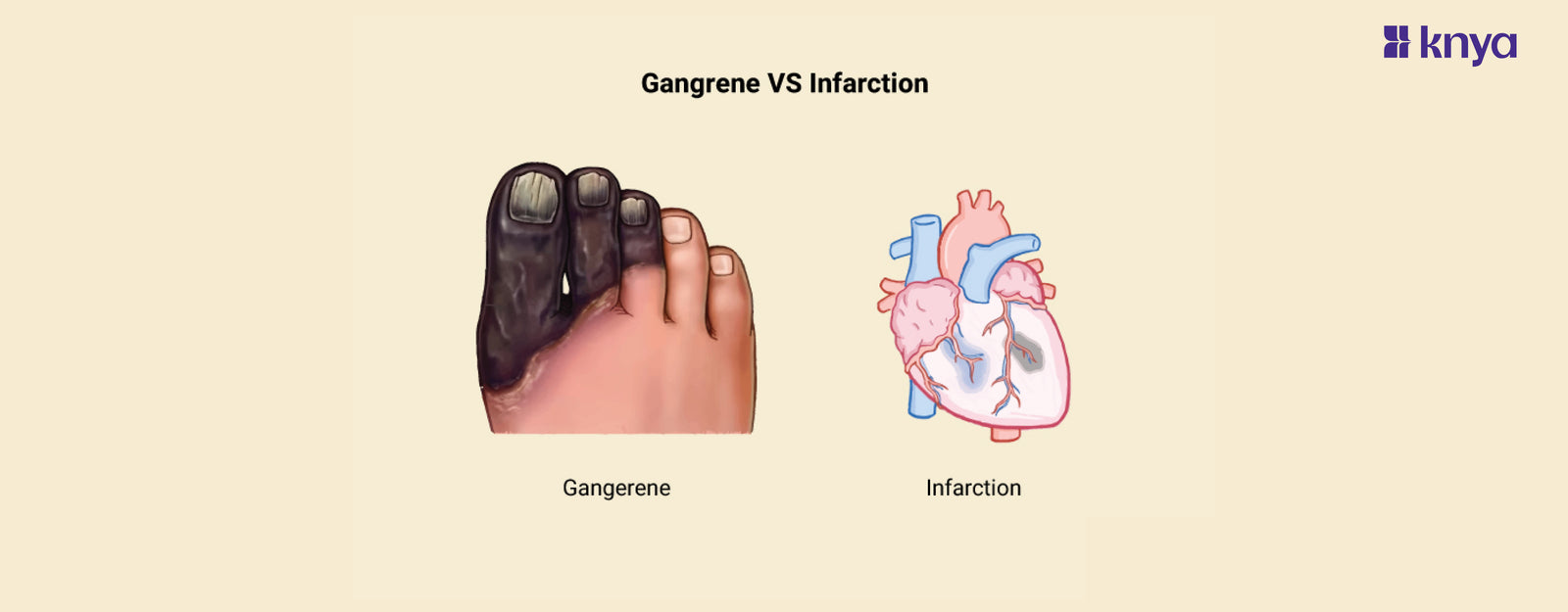
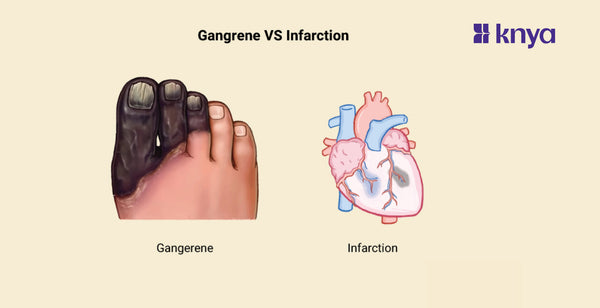
Difference between Gangrene and Infarction: Gangrene and Infarction are both conditions that involve dead tissues. They do differ in terms of the causes and symptoms. Gangrene arises from a lack of blood supply, leading to tissue decay and necrosis, often accompanied by a bacterial infection. It can lead to dry, wet, or gas Gangrene, depending on the presence of infection and moisture levels in the affected area. In contrast, Infarction occurs when blood flow to a specific tissue or organ is obstructed, commonly due to a blood clot or plaque buildup.
Difference Between Gangrene and Infarction
Although both involve tissue degeneration, Gangrene is characterized by impaired blood flow, which could also lead to infection. Infraction is characterized by vascular blockage, which may further lead to tissue ischemia. The table provides the differences between Gangrene and Infarction.
|
Aspect |
Gangrene |
Infarction |
|
Definition |
Death and decay of tissue due to lack of blood supply, often accompanied by infection |
Tissue death resulting from a blockage in blood flow to a specific area or organ |
|
Causes |
Lack of blood supply (ischemia), often due to trauma, diabetes, peripheral artery disease, or infection |
Blockage of blood vessels, typically by blood clots or plaque buildup (thrombus, atherosclerosis) |
|
Types |
Dry, wet, gas gangrene |
Myocardial infarction (heart attack), cerebral infarction (stroke), pulmonary infarction, etc. |
|
Characteristics |
Tissue becomes dry, shrunken, and dark (dry gangrene), or swollen, discolored, and emits foul odor (wet gangrene); may include gas bubbles (gas gangrene) |
Results in tissue ischemia and subsequent necrosis; may lead to permanent damage or dysfunction of affected organ or tissue |
|
Common Locations |
Extremities (especially feet), internal organs, genitals |
Heart, brain, kidneys, lungs, intestines, spleen, limbs, etc. |
|
Associated Symptoms |
Pain, swelling, discoloration, foul odor (in wet gangrene), fever, systemic symptoms (in severe cases) |
Chest pain, shortness of breath, dizziness, weakness, confusion, paralysis (depending on affected organ) |
|
Risk Factors |
Diabetes, peripheral vascular disease, smoking, poor wound care, compromised immune system |
Hypertension, high cholesterol, smoking, obesity, sedentary lifestyle, family history of cardiovascular disease |
|
Diagnosis |
Clinical examination, imaging (X-ray, CT scan, MRI), blood tests (CBC, CRP), tissue biopsy |
Electrocardiogram (ECG), echocardiogram, cardiac enzyme tests (troponin), brain imaging (CT scan, MRI), angiography |
|
Treatment |
Surgical removal of dead tissue, antibiotics (infection), wound care, revascularization procedures |
Medications (thrombolytics, antiplatelet drugs), angioplasty, stent placement, bypass surgery, lifestyle changes, rehabilitation |
|
Prognosis |
Depends on extent of tissue damage, presence of infection, underlying health conditions; can range from minor to life-threatening |
Depends on location and severity; early intervention crucial for minimizing damage and improving outcomes; may lead to complications such as heart failure, stroke, organ failure, or death |
Browse The Best Scrubs Collection!
What is Gangrene?
Gangrene is a serious medical condition that can lead to death and the decay of tissues from a lack of blood flow. It can result in various types, including dry, wet, and gas Gangrene, each with distinct characteristics and complications. This often affects the legs and arms, specifically the toes and fingers.
Types of Gangrene
Gangrene can be classified into mainly three types:
- Dry Gangrene: It occurs when the blood flow to the area is completely stopped. This makes the tissue drier and darker.
- Wet Gangrene: This occurs due to the invasion of bacteria in the tissue, which leads to the sale of the affected area, discoloration, and a foul odor.
- Gas Gangrene: A serious form of wet gangrene caused by a Clostridium bacterium infection that leads to gas bubbles building up in the damaged tissue.
Causes of Gangrene
- Peripheral Artery Disease (PAD): The buildup of plaque in the arteries can restrict blood flow to the extremities, increasing the risk of Gangrene, especially in the legs and feet.
- Diabetes Mellitus: Due to delayed healing of wounds and a weakened immune system, diabetic foot ulcers are more vulnerable to infection and necrosis, which may further lead to Gangrene.
- Trauma: Severe trauma, such as severe burns and accident injuries, can directly destroy blood vessels, resulting in ischemia and tissue death.
- Infection: Dirty or untreated wounds may lead to wet or gaseous gangrene.
- Vascular Disorders: Vascular disorders, including thrombosis (blood clots), embolism (traveling blood clots), or vasculitis (inflammation of blood vessels), can restrict blood flow, predisposing tissues to ischemia and Gangrene.
- Smoking: Tobacco use can damage blood vessels and impair circulation, increasing the risk of peripheral artery disease and Gangrene.
Symptoms of gangrene
- Color change: The area affected may appear red, purple, black, or blue.
- Skin Changes: The skin could get waxy, shiny, or glossy. To the touch, it could also seem chilly.
- Pain: The affected area may experience moderate discomfort or intense, stabbing pain.
- Swelling: Swelling may occur in and around the affected area, often accompanied by tenderness or warmth.
- Foul Smell: In cases of wet gangrene, a foul-smelling discharge may be present due to bacterial infection.
- Ulcers or Sores: Open sores or ulcers may develop on the skin, which can be slow to heal or may not heal at all.
- Blisters: Fluid-filled blisters may form on the skin, particularly in cases of wet gangrene.
Diagnosis and Treatment of Gangrene
The diagnosis of Gangrene usually involves a clinical examination, laboratory tests, and possibly a tissue biopsy to confirm and assess the extent of tissue involvement. Treatment usually involves a combination of methods, including surgical debridement to remove necrotic tissue, antibiotic therapy to treat or prevent infection, revascularization operations to restore blood flow, wound care to encourage healing, and, in certain situations, hyperbaric oxygen therapy.
What is an Infraction?
An Infarction is when tissue dies from a lack of blood flow, usually caused by a blockage or constriction of the arteries supplying the affected area. It usually happens in a specific region of the tissue where blood flow is restricted, which causes ischemia and necrosis.
Types of Infraction
The major types of Infractions are as follows:
- Heart Attack (Myocardial Infarction): This happens when there is an obstruction in the blood supply to a specific area of the heart muscle, usually as a result of a blood clot forming or a coronary artery plaque rupturing.
- Cerebral Infarction (Stroke): Brain tissue is damaged in a cerebrovascular infarction (stroke), which occurs when blood flow to a portion of the brain is interrupted. Blockages in the arteries supplying the brain result in the most common type of stroke, known as ischemic strokes.
- Pulmonary Infarction: This occurs when a blood clot blocks the pulmonary artery or one of its branches, causing tissue death in the lungs.
- Renal Infarction: Causes damage to kidney tissue by obstructing blood flow to a portion of the kidney.
Causes of Infraction
- Atherosclerosis: Atherosclerosis is a disorder that causes blood flow to become narrowed and obstructed due to the accumulation of fatty deposits (plaques) within the walls of arteries. These plaques have the potential to burst, forming blood clots that can obstruct arteries and result in infarctions such as cerebral or myocardial Infarctions.
- Thrombosis: Blood clots that form inside blood vessels are referred to as thrombosis. Thrombi can cause tissue ischemia and Infarction by obstructing blood flow in veins or arteries. Vascular damage, inflammation, and changes in blood clotting mechanisms are among the factors that contribute to thrombosis.
- Embolism: An embolism is a blockage of blood flow caused by a blood clot or foreign objects (such as fat, air, or tumor cells) that enter a blood vessel through the bloodstream and lodge there. Embolisms can start in far-off places, including the heart (as in atrial fibrillation or heart valve problems) or the legs' deep veins (as in deep vein thrombosis), and they can spread to different organs, causing infarction.
- Trauma: Tissue ischemia and infarction can result from physical harm or trauma to blood vessels, which can interrupt blood flow. This can happen in several situations, including penetrating injuries, acute trauma, and surgical complications.
Symptoms of Infarction
The symptoms of each Infraction are different from others, to mention a few.
- Heart Attack (Myocardial Infarction): Symptoms include chest pain or discomfort, pain or discomfort in the arms, back, neck, jaw, or stomach, shortness of breath, nausea, vomiting, cold sweats, and weakness.
- Cerebral Infarction (Stroke): Symptoms include sudden weakness or numbness, difficulty speaking or understanding, vision problems such as blurred vision, severe headache, loss of balance or coordination, and dizziness.
- Pulmonary Infarction: Symptoms include sudden onset of sharp chest pain, shortness of breath, coughing up blood (hemoptysis), rapid heart rate (tachycardia), and fever.
- Renal Infarction: Symptoms include severe flank or abdominal pain, nausea, vomiting, blood in the urine (hematuria), fever, fever, and chills.
Diagnosis and Treatment
Diagnosis includes examining medical history, physical examination, and imaging tests like ECG, echocardiography, CT, MRI, and angiography. Revascularization procedures like thrombolytic therapy, angioplasty, or surgery to restore blood flow, medications, oxygen therapy, and pain management are a few treatments for Infraction.
Both involve tissue death due to compromised blood supply and share risk factors, including diabetes, peripheral artery disease, and atherosclerosis. They may share common symptoms, but they are different in many ways. If left untreated, both can be fatal.
Order the Best Jogger Scrub From Here!
| Check out More Articles | |
| Difference Between Tendon and Ligament | |
| Difference Between Seizure and Epilepsy | |
| Difference Between Hypothyroidism and Hyperthyroidism | |