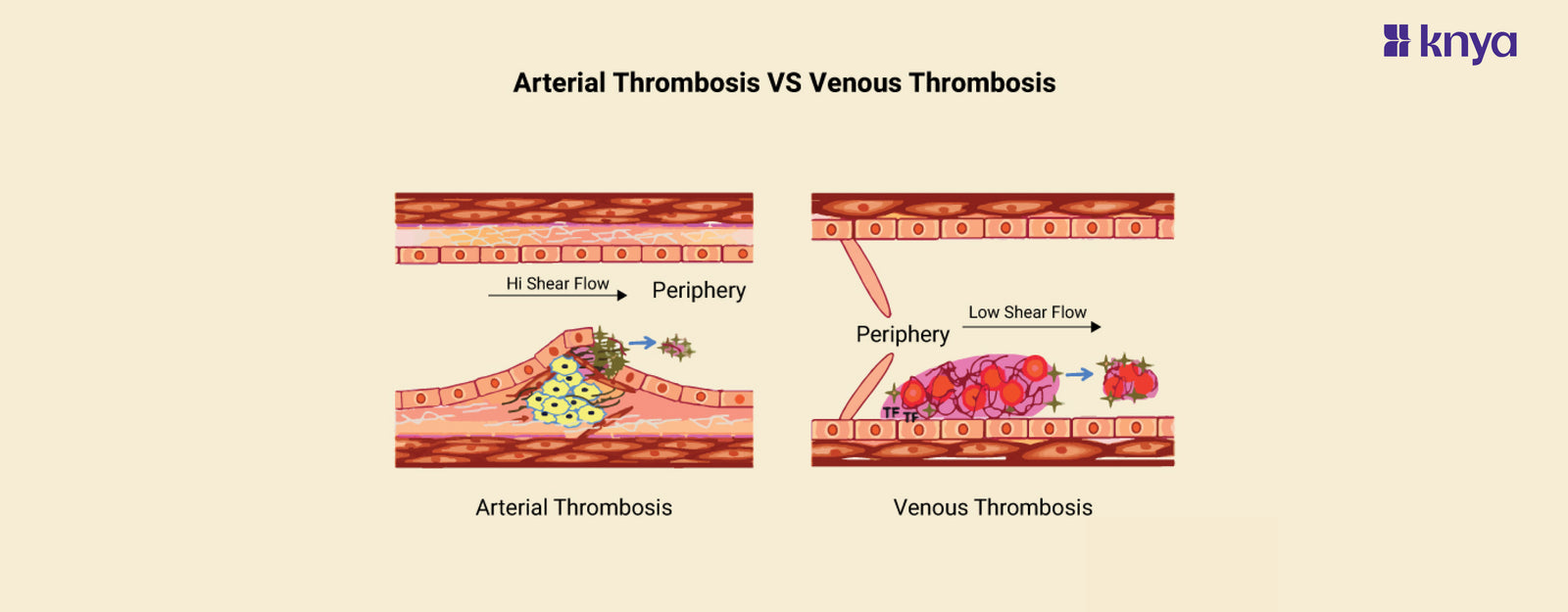
Arterial Thrombosis and Venous Thrombosis involve blood clots blocking vessels, but with key differences. Arterial Thrombosis occurs in arteries, carrying oxygen-rich blood away from the heart, and often results from plaque buildup (atherosclerosis). This can lead to heart attacks, strokes, and limb ischemia. Venous Thrombosis, on the other hand, affects veins returning blood to the heart, commonly due to slow blood flow and often starting in the legs (Deep Vein Thrombosis). While less immediately life-threatening, it can dislodge and travel to the lungs (Pulmonary Embolism) causing serious harm. Arterial Thrombosis Vs Venous Thrombosis highlights the critical distinction in vessel type, underlying cause, and potential consequences, emphasizing the need for accurate diagnosis and targeted treatment. Remember, consulting a healthcare professional is crucial if you suspect either condition.
Difference Between Arterial Thrombosis and Venous Thrombosis
Arterial thrombosis and venous thrombosis are both blood clotting illnesses, although they affect separate regions of the circulatory system and have unique features. Here are the key differences between arterial and venous thrombosis.
|
Aspect |
Arterial Thrombosis |
Venous Thrombosis |
|
Location |
Arteries |
Veins |
|
Blood Flow |
Complete blockage |
Partial obstruction |
|
Causes |
Atherosclerosis, arterial injury |
Stasis of blood flow, vascular injury, hypercoagulability |
|
Risk Factors |
Hypertension, high cholesterol, smoking, diabetes |
Prolonged immobility, surgery, pregnancy, inherited clotting disorders |
|
Symptoms |
Sudden and severe symptoms (e.g., chest pain, limb numbness) |
Leg pain, swelling, warmth |
|
Complications |
Heart attack, stroke, limb ischemia |
Deep vein thrombosis (DVT), pulmonary embolism (PE) |
|
Treatment |
Antiplatelet drugs, anticoagulants |
Anticoagulant therapy, compression stockings |
|
Prognosis |
More severe consequences |
Usually less immediately life-threatening |
|
Prevalence |
Less common |
More common |
|
Prevention |
Lifestyle modifications, managing risk factors, medication adherence |
Early mobilization after surgery, compression stockings, prophylactic anticoagulation |
Browse Best Scrubs Collection
What is Arterial Thrombosis?
Arterial thrombosis occurs when a blood clot develops in an artery, impeding the flow of oxygenated blood to essential organs. This can result in significant complications such as a heart attack, stroke, or even death. The most prevalent cause of arterial thrombosis is atherosclerosis, a disorder characterised by the accumulation of fatty deposits in the arteries' walls. Other risk factors include high blood pressure, elevated cholesterol, smoking, and diabetes.
Key Features of Arterial Thrombosis:
- Arterial thrombi form in arteries, the blood vessels carrying oxygen-rich blood away from the heart to organs and tissues.
- Atherosclerosis, or plaque formation in arterial walls, is frequently the cause. Plaque rupture can expose underlying tissues, causing platelets and clotting components to form a thrombus. Other factors include high blood pressure, diabetes, smoking, and certain drugs.
- Can result in ischemia events (tissue and organ damage caused by blood flow obstruction). Examples include heart attack (coronary artery thrombosis), stroke (cerebral artery thrombosis), and peripheral artery disease (blockage of leg arteries).
- Depending on the afflicted artery and its severity. Common symptoms include acute pain, numbness, weakness, and trouble speaking or moving (depending on location).
What is Venous Thrombosis?
Venous thrombosis occurs when a blood clot forms in a vein, typically in the legs. This can cause pain, swelling, and redness in the affected area. If the clot breaks loose and travels to the lungs, it can cause a pulmonary embolism, which is a life-threatening condition. Risk factors for venous thrombosis include surgery, prolonged immobility, pregnancy, and certain medical conditions.
Key Features of Venous Thrombosis:
- Venous thrombi form in veins, the vessels carrying oxygen-depleted blood back to the heart.
- Slow blood flow (stasis), vessel wall damage (endothelial dysfunction), and an increased risk of clotting (hypercoagulability). Prolonged sitting/immobility, surgery, certain drugs, and genetic disorders are all potential contributors.
- The most frequent kind is deep vein thrombosis (DVT), which often occurs in leg veins. DVT can break off and move to the lungs, resulting in a potentially fatal pulmonary embolism (PE). Other problems include chronic venous insufficiency and post-thrombotic syndrome.
- DVT can result in leg edoema, discomfort, redness, and warmth. PE symptoms include shortness of breath, chest discomfort, and bloody cough.
Order the Best Jogger Scrub from Here!
Similarities between Arterial Thrombosis and Venous Thrombosis
- Arterial and Venous thrombosis entail the production of blood clots (thrombi) within the blood arteries.
- Both are caused by abnormalities in the balance of coagulation and anticoagulation components, which result in aberrant clot formation.
- Both forms of thrombosis increase the risk of embolisation, which occurs when fragments of the clot break off and move through the circulation, blocking smaller veins.
- Both arterial and venous thrombosis frequently need long-term treatment to avoid recurrence and manage accompanying problems.
- Diagnostic methods such as ultrasound, CT scans, MRI, and blood tests (D-dimer, coagulation studies) are used to identify and confirm arterial and venous thrombosis.
Arterial thrombosis and venous thrombosis both include blood clots that develop within vessels, but they differ greatly in location, aetiology, and outcome. Arterial thrombosis occurs in the arteries, which carry oxygen-rich blood away from the heart, and is commonly caused by plaque formation (atherosclerosis). This can cause heart attacks, strokes, and limb ischemia. Venous thrombosis, on the other hand, affects the veins responsible for returning deoxygenated blood to the heart and is often caused by factors such as extended immobility or certain drugs. It often manifests as deep vein thrombosis (DVT) in the legs, with the potentially fatal consequence of pulmonary embolism if the clot breaks free and goes to the lungs. Understanding these distinctions is critical for correct diagnosis, appropriate management, and avoiding major problems caused by each form of thrombosis.
Explore All Women's Scrub
| Check out More Articles | |
| Difference Between Cartilage and Bone | |
| Difference Between Endocrine and Exocrine Glands | |
| Difference Between Cell Wall and Cell Membrane | |