Differences Between Ankylosing Spondylitis and Rheumatoid Arthritis: When it comes to inflammatory joint diseases, two conditions that often come to mind are Ankylosing Spondylitis (AS) and Rheumatoid Arthritis (RA). While both are autoimmune disorders that affect the joints, they have distinct characteristics, symptoms, and treatment approaches. Understanding the differences between these conditions is crucial for accurate diagnosis and effective management.
Differences Between Ankylosing Spondylitis and Rheumatoid Arthritis
The differences between ankylosing spondylitis and rheumatoid arthritis are discussed below.
| Feature | Ankylosing Spondylitis (AS) | Rheumatoid Arthritis (RA) |
| Joint Affected | Primarily axial skeleton (spine, SI joints) | Small and large joints, symmetrical involvement |
| Extra-Articular Manifestations | Uveitis, cardiac involvement, lung involvement | Rheumatoid nodules, vasculitis, pulmonary involvement |
| HLA-B27 Association | Strong association (over 90% HLA-B27 positive) | Variable association with RF and anti-CCP antibodies |
| Age of Onset | Typically starts before age 30 | Peak onset between ages 30 and 50 |
| Morning Stiffness | Improves with exercise, can last several hours | Lasts more than an hour, often severe in the morning |
| Symmetry of Joint Involvement | Asymmetrical | Symmetrical |
| Treatment Approach | Focuses on reducing inflammation, preserving mobility | Aims to suppress inflammation, prevent joint damage |
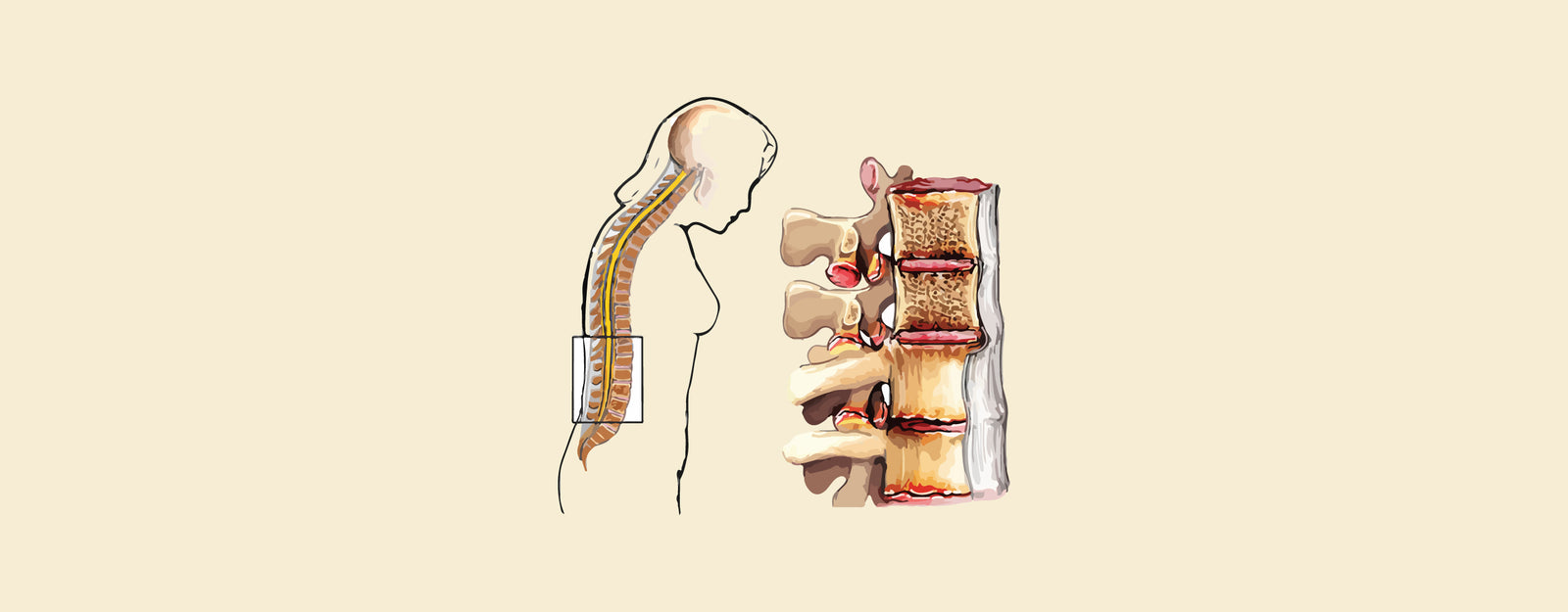
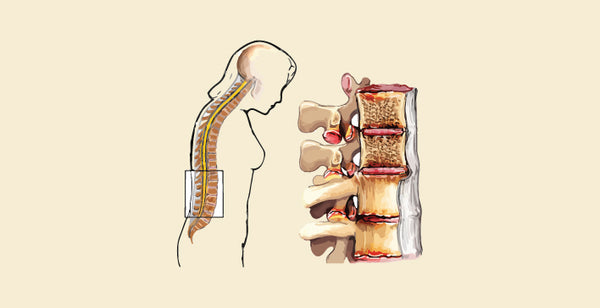
What Is Ankylosing Spondylitis (AS)?
Ankylosing Spondylitis is a chronic inflammatory disease primarily affecting the spine and sacroiliac joints. It belongs to a group of conditions known as spondyloarthritis, which also includes psoriatic arthritis and reactive arthritis. AS primarily affects young adults, typically presenting in late adolescence or early adulthood. Here are the key features of AS:
Key Features of Ankylosing Spondylitis
Symptom Onset:
- Symptoms usually begin in early adulthood, often before the age of 30.
- Initial symptoms may include chronic lower back pain and stiffness, which worsen with rest and improve with exercise.
- Fatigue and discomfort in other areas such as the hips, shoulders, and heels may also occur.
Joint Involvement:
- Predominantly affects the axial skeleton, including the spine and sacroiliac joints.
- Can lead to bamboo spine, a condition characterized by fusion of the vertebrae, resulting in decreased mobility.
- Peripheral joint involvement may occur in later stages of the disease, affecting joints such as the hips, shoulders, and knees.
Extra-Articular Manifestations:
- AS can involve extra-articular structures such as the eyes (uveitis), heart, and lungs.
- Uveitis is a common complication, presenting as eye pain, redness, and sensitivity to light.
- Cardiovascular complications may include aortitis and aortic valve insufficiency.
HLA-B27 Association:
- Strong association with the HLA-B27 gene, found in over 90% of individuals with AS.
- Presence of HLA-B27 may influence disease severity and progression.
- However, not all individuals with HLA-B27 develop AS, indicating the involvement of other genetic and environmental factors.
Treatment Approach:
- Treatment focuses on reducing inflammation, managing symptoms, and preserving mobility.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used as first-line therapy to alleviate pain and stiffness.
- Disease-modifying antirheumatic drugs (DMARDs) such as tumor necrosis factor (TNF) inhibitors may be prescribed for individuals with persistent symptoms and evidence of spinal damage.
What Is Rheumatoid Arthritis (RA)?
Rheumatoid Arthritis is a systemic autoimmune disease characterized by chronic inflammation of the synovial membrane, leading to joint destruction and deformity. Unlike AS, which primarily affects the spine, RA can involve multiple joints throughout the body. Here are the key features of RA:
Key Features of Rheumatoid Arthritis
Symptom Onset:
- Symptoms often begin between the ages of 30 and 50, although RA can occur at any age.
- Symmetrical joint involvement is characteristic, with morning stiffness lasting more than an hour.
- Generalized symptoms such as fatigue, fever, and weight loss may accompany joint manifestations.
Joint Involvement:
- RA typically affects small joints first, such as those in the hands and feet, before progressing to larger joints.
- Joint inflammation can lead to erosion of cartilage and bone, causing deformities and functional impairment.
- Rheumatoid nodules may develop in areas of repeated pressure, such as the elbows and fingers.
Extra-Articular Manifestations:
- RA is associated with various extra-articular manifestations, including rheumatoid nodules, vasculitis, and pulmonary involvement.
- Rheumatoid nodules are firm, non-tender masses that can develop under the skin, most commonly over bony prominences.
- Rheumatoid vasculitis may affect small and medium-sized blood vessels, leading to skin ulcers, neuropathy, and organ damage.
Rheumatoid Factor and Anti-CCP Antibodies:
- Most individuals with RA test positive for rheumatoid factor (RF) and/or anti-cyclic citrullinated peptide (anti-CCP) antibodies.
- These autoantibodies are useful in diagnosing RA and assessing disease severity.
- However, seronegative RA, characterized by the absence of RF and anti-CCP antibodies, also exists, particularly in early disease stages.
Treatment Approach:
- Treatment aims to suppress inflammation, alleviate symptoms, and prevent joint damage.
- Disease-modifying antirheumatic drugs (DMARDs), biologic agents, and corticosteroids are commonly used to manage RA.
- Early and aggressive treatment with DMARDs has been shown to improve long-term outcomes and reduce the risk of irreversible joint damage.
Similarities Between AS and RA
- Autoimmune Origin: Both AS and RA are autoimmune diseases characterized by immune system dysfunction.
- Chronic Inflammation: Both conditions involve chronic inflammation of the joints, leading to pain, stiffness, and functional impairment.
- Systemic Manifestations: Both AS and RA can affect various organ systems beyond the joints, leading to extra-articular complications.
| Check out More Articles | |
| Difference Between Cartilage And Bone | |
| Difference Between Endocrine And Exocrine Glands | |
| Difference Between Cell Wall And Cell Membrane | |